Parkinson’s disease clinical trials: Challenges, advancements, and the role of technology

The ability to use technology as a novel digital endpoint becomes especially important in diseases where mobility is impaired, such as in Parkinson’s disease (PD) – an area in which there have been several recent achievements.
To explore these advancements, as well as the challenges to PD research, Outsourcing-Pharma (OSP) spoke with two central nervous system (CNS) experts from the contract research organization (CRO) Icon: Peter Schueler, senior vice president, drug development services (PS) and Haichen Yang, vice president, global therapeutic lead (HY).
OSP: What are some of the main challenges specific to Parkinson’s disease trials?
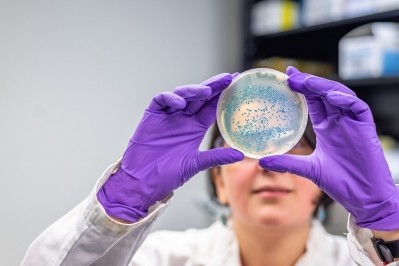
PS: Patients suffering from a movement disorder such as PD are limited in their ability to travel to any study center. Fewer activities at the sites and more assessments at the patient’s home are an appropriate approach to limit patient burden.
Novel digital (wearable) technologies as alternative study endpoints facilitate this approach. Another limitation is the lack of yet existing registries for patients “at risk” for PD. Similar registries allowed the enrollment of prodromal patients in recent AD studies, and a similar “treat early” concept may become necessary when developing PD disease-modifying therapies (DMTs).
HY: As the field is moving toward developing DMTs, clinical studies have to rely more on biomarkers and imagining to assess disease progression and treatment effects. Developing good tracer and imaging technology for PD become a pressing need.
On the other hand, it can be challenging to get consent from prodromal and early-stage PD patients to give CSF samples for biomarker assessments in clinical trials.
OSP: What recent advancements have been made in this area?
PS: As a major achievement, alpha-synuclein was identified as a potential target for a disease-modifying therapy. However, there is some similarity with beta-amyloid, which was targeted for Alzheimer’s. Thus, an engagement with that target alone will not yet guarantee clinical effectiveness.
Another interesting new concept is the potential role of our microbiome as a trigger for PD (and potentially other neurodegenerative diseases). Further prospective studies in that field may help to develop more targeted and earlier treatments.
OSP: What role has technology played?
PS: The assessment of movement via miniaturized gyroscopes was initially developed for smartphones (e.g. to auto-rotate the screen). It was easily transferred in dedicated wearables to assess tremor, rigor, micrography and gait abnormalities as key symptoms of PD.
In near future, these “digital” endpoints will be adequately valid to be used as primary endpoints, allowing the assessment of PD symptoms over longer periods of time and a more naturalistic (patient’s home) environment. That should improve the sensitivity of the assessments and as a consequence also study power.
OSP: More generally, what are the challenges to neurological trials?
PS: Unfortunately, the human brain is the most complex structure in the universe (as we know it). The underlying pathophysiology are understood more and more – but by far not fully. That is in contrast to more singular models such as infectious diseases or oncology, where the outcome can often get measured and observed in single cell lines ex vivo.
Steadily growing computer processing power does help with some modeling in CNS research, but will most probably never allow for a full explanation of the expected outcome.
HY: Vast majority of neurological disorders are considered as chronic conditions and needed for long-term treatment. Therefore, the duration of clinical trials has to be sufficiently long to assess efficacy and safety for chronic use.
Development timeline for neurological drugs are usually long. Blood brain barrier provides a protective layer for human brain against toxic substances and microorganism.
To develop new drugs for neurological disorders, chemical entities and/or large molecules have to be able to penetrate or by-pass the blood brain barrier, adding another level of complexity.
How does study design affect patient enrollment and retention? And how can this be improved?
PS: With new treatment strategies targeting early or even pre-symptomatic stages of the disease, “patients” are no longer the target population. It will be individuals who are either completely healthy or only suffer very mild initial symptoms – often too mild to trigger a diagnosis.
It will thus be needed to identify such individuals “at risk” based on their genetic profile (in biobanks) or other risk factors, such as sick family members.
The required (re-)identification of such subjects “at risk” will create more debates about data privacy. It also necessitates new screening and enrollment strategies, e.g. through motor performance assessments with smartphone apps.
However, the option to recognize various (motor) symptoms early in combination with a known genetic risk profile will enable a coming generation of patients to much earlier seek for a modifying therapy – or simply adjust their lifestyle to reduce the risk.
HY: The design of clinical trials evaluating DMT can be complicated. To assess disease progression and drug effects, various CSF biomarkers and imaging markers are needed in addition to standard clinical endpoints. Sufficient study duration is necessary to detect sustained divergence in outcome measure between groups over time.
A post-treatment observation period could demonstrate a sustained divergence in symptoms between originally active and placebo-treated groups. All those design elements can affect patient enrollment and retention.
Researchers should strive to include only those necessary endpoints, reduce the frequency for follow-up visits and consider using technologies and home visits.